Alternate Approaches to Developing a Malaria Vaccine
Dr Anusha Munasinghe Gunasekera (1996) read Natural
Sciences at Clare, followed by a PhD in malarial molecular biology
at Harvard University, USA.
Her post-doctoral fellowship at the Harvard School of Public
Health, USA, was conducted partly in Sri Lanka in collaboration
with the Malaria Research Unit, University of Colombo.
She joined Sanaria Inc in 2006, a biotechnology firm at the
forefront of malarial vaccinology, where she currently serves as
Senior Advisor, Regulatory Affairs. Here she shares some of the
results from over a decade of whole parasite vaccine development.
My introduction to the complex yet fascinating field of malariology began during the summer of my second year at Clare. I undertook an internship at the Malaria Research Unit, Sri Lanka, to fulfill the independent research requirement of the part II Natural Sciences Tripos. At the time, I had no idea that this was just the beginning of a life-long calling to tackle this deadly mosquito-borne disease.

Salivary gland harvest team
Salivary gland harvest team
We, in the malaria community, are only too well aware of the grim statistics – 247 million cases, and 619,000 deaths in 2022, mostly caused by the parasite, Plasmodium falciparum, in young children in sub-Saharan Africa. But as researchers, how many of us have the opportunity to try to directly impact the very numbers used to justify our grants, proposals, and regulatory dossiers?
I received just such an opening upon joining Sanaria Inc, a biotechnology firm in Maryland, USA, headed by Dr Stephen L. Hoffman, who has approached vaccinology from various angles for decades. Sanaria is developing a whole organism vaccine based on the P. falciparum sporozoite (PfSPZ); PfSPZ initiates infection in the human liver after injection by mosquito carriers. PfSPZ in Sanaria’s vaccines, however, are alive but weakened, so that they can safely elicit an immune response, without causing disease.
The preferred product characteristic of a successful malaria vaccine, as recently defined by WHO, is one with vaccine efficacy (VE) of at least 90% against clinical malaria/infection in the field; VE is a measure of how much a vaccine lowers risk of getting sick. The realization of such a vaccine has long been hampered by lack of funding, as well as Plasmodium’s complicated life cycle and ability to alter its surface molecules. Known as antigenic variation, the latter permits Plasmodium to evade host immunity. Thus despite concerted efforts spanning 50 years, there remain only a few promising vaccine candidates to date, including RTS,S/AS01E (VE of ~ 30% against clinical pediatric malaria). We hope that Sanaria’s whole organism approach will help circumvent some of the issues faced by subunit vaccines that focus on single antigens.
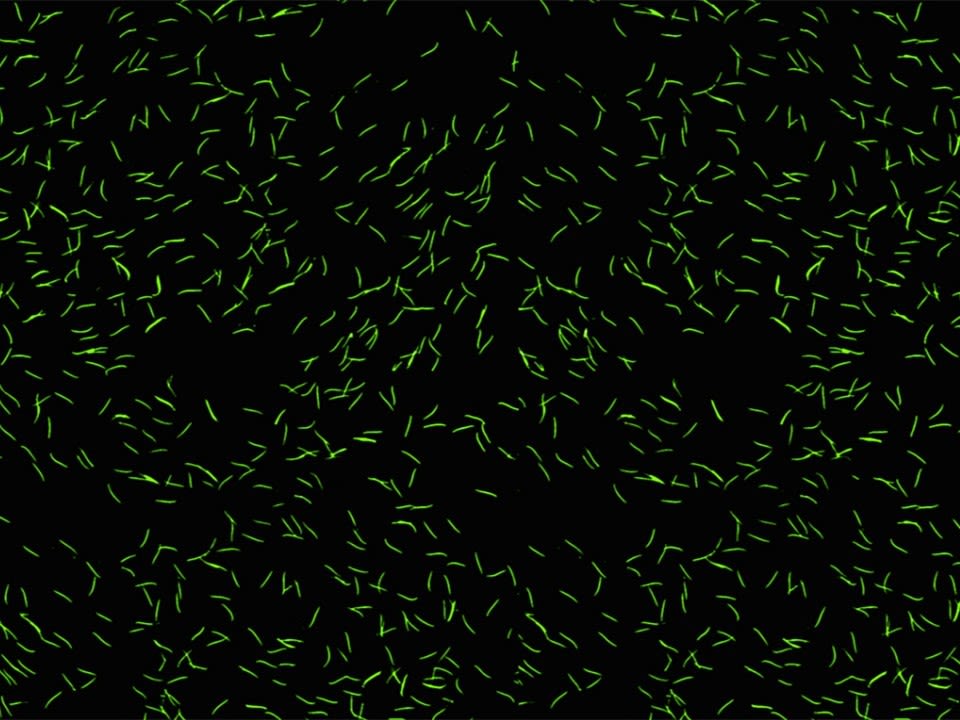
Towards this end, Sanaria developed new technologies to remove PfSPZ from inside the mosquitoes’ salivary glands, clean them up and bottle them in a form that can be preserved long term, easily transported, and safely injected into humans. In our first-generation vaccine, infected aseptic mosquitoes are irradiated to weaken the parasite within, and salivary glands are harvested manually to release PfSPZ, which are then purified, counted, and cryopreserved to produce PfSPZ Vaccine. In addition, Sanaria has demonstrated that the vaccine is sterile, adequately weakened, but potent, following quality control release testing.
When I joined Sanaria in 2006 as a research scientist, the company was still growing, requiring me to wear multiple hats: from pain-staking, head-to-toe sterile gowning procedures required to enter ISO standard clean rooms for manufacturing; to tedious teasing of parasites from the insect salivary glands using a fine needle; to administration of PfSPZ Vaccine in pivotal animal studies required to demonstrate safety prior to human injection.
Working on so many different phases of vaccine development ultimately prepared me for the challenging role of heading our newly formed Regulatory and Clinical Affairs division in 2008, which required overseeing clinical trials across the globe, and interacting with numerous regulatory bodies (US FDA, EU EMA, CCMO in the Netherlands, German PEI, and Tanzanian FDA). In February 2009, after submitting our first regulatory dossier to the FDA - an Investigational New Drug for the first ever whole-cell eukaryotic vaccine produced under current Good Manufacturing Practice - I felt as though I had given birth, even though my son was not due until later that year!
The decade that followed witnessed the expansion of our clinical program to over 40 trials worldwide that involved three products (radiation-, chemo- and genetically-attenuated PfSPZ). After a few hiccups to iron out issues such as route of administration and dosing regimen, Sanaria’s vaccine portfolio demonstrates both an exceptional safety profile (safely administered in 5-month to 61-year olds), and excellent VE (VE of upto 90% following controlled exposure and upto 62% in the field, with radiation-attenuated vaccine). Of note, the achievement of 100% VE against controlled exposure with chemo-attenuated PfSPZ, suggests we may be close to fulfilling the need for that highly efficacious vaccine called for by WHO.
In closing, I wish to acknowledge what an immense privilege studying at Clare was. Certainly, my time there laid the foundation and gave me the training to pursue higher studies in infectious diseases. This afforded me the chance to work with only the “greats” in the field - Prof Kamini Mendis (formerly WHO) at Colombo University, who introduced me to malariology, Prof Dyann Wirth, my PhD advisor at Harvard, who refined and polished my skills, and finally Dr Hoffman at Sanaria, who helped put my knowledge to practical use.

Anusha with Dr Hoffman and family
Anusha with Dr Hoffman and family
